Resurfacing or still drowning in despair?
A brief commentary on Andy Murrays new documentary “Resurfacing”
https://www.imdb.com/title/tt11243364/
I initially watched Andy Murray’s “Resurfacing” documentary out of curiosity due to some twitter comments and recommendations to watch it . I didn’t expect it to be so engrossed and at some points emotionally involved in Murray’s journey. I also found myself questioning some of the wisdom of the medical interventions, rehab and medical advice he received. That said, I accept that it’s easy to be critical and that hindsight is often 20/20.
After tweeting a few comments it was suggested maybe I should write a blog review. So I did.
Problem is I started the blog several times then deleted it. Below is my fourth effort, enjoy.
I re-watched “Resurfacing” wrote some notes during the documentary and still don’t quite know what to make of Murray’s whole journey.
I recommend that readers watch the documentary (if they have access) and make up their own minds. One good thing to come out of watching the documentary twice and reflecting on my thoughts about what occurred over two years, was I had to read some new evidence based papers on corticosteroid injections in to the hip (which fueled a great discussion on twitter here https://twitter.com/retlouping/status/1213466336426369036?s=21 ), and MRI findings in the hips of high level athletes, and one on findings in asymptomatic individuals compared to age and sex matched symptomatic patients, which I reviewed on twitter here https://twitter.com/retlouping/status/1213524327125135360?s=21 and here https://twitter.com/retlouping/status/1213794544648704000?s=21
The documentary starts with Murray preparing for surgery on his right hip. He has a long history of right hip issues but in January 2018 he made the decision to have arthroscopic surgery to “fix” his hip issues that have not “healed” with conservative care.
On January 9th 2018 Murray undergoes arthroscopic hip surgery, reports post surgery by Murray indicate he had a torn ligamentum Teres which was trimmed, a repair of a torn labrum, cleaning up of “inflamed tissue” and the surgeon noted excessive articular cartilage damage. (Remember this as it is important later)
Post op Murray and his medical/ rehab team, which compromised two Physiotherapists, a conditioning trainer, a Pilates instructor, and his tennis coach, did lots of passive stretching, pool work, strength and conditioning including bike work, reformer and climber.
Jamie Delgado, Murray’s coach, states a few weeks after the surgery “Surgery went well, it got rid of the issues.”
Murray’s team were focusing on a quick return to function and improved range of motion. The biggest issue was Murray’s function was apparently progressing well, the only thing that wasn’t progressing was his PAIN.
In Murray’s own words his hip felt “sore and weak.” Despite lots and lots of hard work and strength training.
A comment that made the hairs stand up on the back of my neck was “We didn’t know how long it would take to recover from the surgery.”
How could this be possible?
My observation was that Murray was doing too much too soon in his post op rehab and was not respecting the repair and healing process. Too much passive stretching, not considering post op movement restrictions such as external hip rotation in the early phase of labral repair surgery.
Of course Murray was painful, his body was still recovering from what is major surgery. I think he and his team made the mistake of thinking minimally invasive arthroscopic surgery means minor surgery due to small wounds. They also seemed to be under the impression that Murray’s hip was ‘fixed” and it was just a matter of getting his conditioning back. I think they did not respect his post op pain enough.
In April 2018 Murray was still having a lot of pain in his right hip, so they consulted a new MD who advised them to have a repeat MRI and consider pain management strategies including oral medication, cortisone injections and nerve ablation to “numb down” the hip to allow Murray to push harder on returning to play.
Quote “once you get rid of the pain and improve the range of motion, then it’s down to the rehab team”
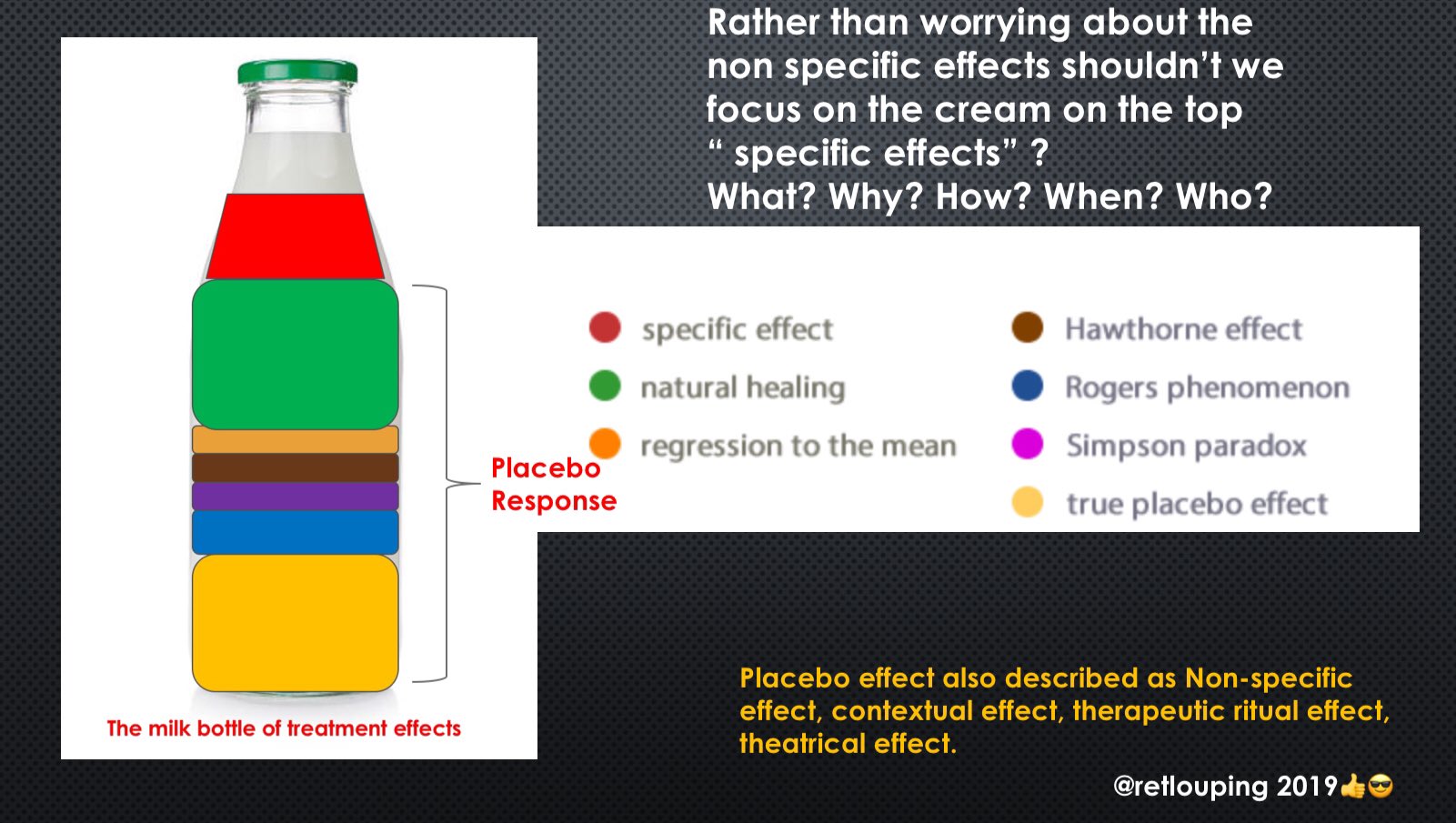
Over the next few months Murray had two intra-articular cortisone injections and two nerve ablation procedures. As expected he had some improvement in his pain and he started to ramp up his training, conditioning and tennis practice. He continued to “push through the pain” but continued to have ongoing hip pain when he tried to practice tennis at full steam.
My thought at this point were why would you numb the area that is obviously causing problems under high mechanical load, so that you could go ahead and expose that area to more high mechanical load?
This is akin to having a sore forehead from repeatedly smashing your head against a wall, the solution isn’t numb your forehead to allow you to keep smashing your head against the wall?
Plus what is the risk on of accelerating the articular cartilage defects noted at Murray’s arthroscopic surgery? I refer back to the twitter thread on this https://twitter.com/retlouping/status/1213466336426369036?s=21
Was it wise to have the corticosteroid injects?
Was it wise to have the nerve ablations?
(Remember hindsight is 20/20 but did his medical team consider the risks, rewards and the evidence?)
In August 2018 Murray decides to return to tennis to test out his hip out. He plays and wins two extremely long matches. In his third match he is visibly struggling with hip pain, he is limping and struggling to go for shots that require high loads through the right hip. Murray is visibly despondent and crying after the match.
Murray comments post match “my body doesn’t want to do it, my mind doesn’t want to push through the pain barrier.” He is visibly distressed. “My body is telling me NO, it hurts.”
August 2018 Murray appears physically and mentally spent. His wife Kim discusses trying to continue and commit to carrying on until the end of the year.
It’s at this point you realize that Murray is not just a Tennis player, he is a brand and an Industry, he employs a host of people and has responsibilities to sponsors. Retiring has big personal and financial repercussions.
Murray decides to try something with different energy?
After watching the documentary twice I realized that Murray is obviously bombarded with solicited and unsolicited advice from many sources. He receives mail on a daily basis offering him advice and “medical fixes” for his problem.
He also echos that every time he engages with a new practitioner he gets new hope, which is dashed when the new approach doesn’t work. I pondered that no where in the documentary did we see Murray receive any professional psychological support?
In August 2018 Murray travels to Philadelphia to try a new rehab approach with Bill Knowles at YSC sports. At YSC Murray undergoes a series of new rehab exercises including break dancing, playing like a child, forward rolling, leap frogging. The idea seems to be to return to simple play patterns to distract Murray and move his hip in unfamiliar patterns. The approach also involves manual therapy and “alignment” of his spine and hip. At the end of the therapy Murray seems somewhat frustrated that he is still in pain.
“Every single brings hope and a flicker that this is it.”
“None of the therapy is done in bad faith.”
December 2018 Murray is practicing on court in Miami. Murray seems to be reaching his psychological low.
Quote:
“There is nothing I can do.”
“I want someone to say stop.”
“I feel like I don’t deserve this. I literally have done everything I have been told.”
“I feel like I deserve a better outcome.”
It appears at this stage that Murray has lost his internal locus of control.
Murray discusses that he will perhaps play in the 2019 Australians open and retire at the 2019 Wimbledon tournament if he can stay match fit through the pain.
We see Murray play and loose his first round singles match at the Australian open, where in an emotional interview he appears bid farewell to tennis
There is a light hearted moment at this stage of the documentary where Marry is seen collecting the days mail and limping visibly jokes about the unsolicited letters he receives from people offering to “fix” his hip.
“Ah! this one is asking if I have considered the homeopathic remedy.” (Chuckles out loud)
Murray decides to retire than decides not to, he is tracking, with interest, the the return to tennis of Bob Bryan who has undergone a hip resurfacing surgery and returned to high level doubles tennis. We see Murray reviewing videos of hip resurfacing and discussing a possible early surgery and a return to tennis at Wimbledon.
He is seen working out on his climber and receiving news that his resurfacing surgery will be on January 28th. He verbalizes that he has no doubts about the surgery but wants it ASAP as he may second guess his decision and he keeps getting messages from other surgeons, saying go with them.
On January 29th 2019 Murray undergoes a hip resurfacing procedure of his right hip.

Side note on the perils of SoMe:
Murray posts pictures of him in bed, post surgery and X-rays of his hip resurfacing on instagram. Both pictures cause heated discussion and some humor on SoMe.
The X-ray has numerous comments because Murray’s genitals are visible on the X-ray.
The picture of him in his bed starts a heated debate and arguments amongst doctors in the USA and UK due to the drip, cannula and blood pressure cuff placement on Murray’s arm. (He is a right handed tennis player)
https://www.avainfo.org/page/AndyMurray
Despite the SoMe controversy the recovery from his hip resurfacing went well.
Murray asks his surgeon if he can return to tennis without damaging his new hip, his surgeon says he has a 15% chance of destroying the resurfacing over seven years if he does. Apparently Murray was comfortable with the risk.
My observation was that post hip resurfacing Murray’s rehab was much more measured an appropriate. He didn’t over do things, he followed a graded loading program with less passive stretching a more self directed activities from pool therapy to land exercises. His rehab was also much more prolonged and he didn’t return to tennis drills until 4 months post surgery, in contrast after his initial labral repair surgery he had been pushing his rehab and tennis hard in the hope of a quick return.
Murray also appeared to be much more comfortable in his own skin and was enjoying being pain free for the first time in several months. He even questioned whether he wanted to commit to the work required to return to first class tennis, he appeared to be enjoying family life and just being able to go about his day without hip pain.
In May 2019 he returned to active on court tennis practice and did some measured sprints which looked free and easy and were at a speed far above his previous levels for the past 12 months. He is seen discussing returning to high level tennis with his surgeon, who jokingly asks if she needs to buy a hat to come watch him at Wimbledon?
“Carry on” remarks his surgeon.
The documentary ends on an extremely high note with Murray returning to Doubles at queens with Lopez and they win the tournament. Murray’s return to tennis is complete????
As I write Murray has played several singles matches in 2019 everything seemed on track for him to play singles in the Australian open in 2020.
Sadly Murray has announced that he has withdrawn from the Australian open due to a “pelvic injury” it has been reported he has a bone bruise of his pelvis on the side of his hip resurfacing.
Andy Murray Out Of Australian Open Because Of Pelvic Injury
https://www.forbes.com/sites/daniellerossingh/2019/12/28/andy-murray-out-of-australian-open-because-of-pelvic-injury/
Is this an early sign of overload and a warning sign for Murray’s future? Only time will tell.
Overall the documentary is an emotional rollercoaster ride for both Murray and the watcher. As a medical practitioner it is sometimes hard to watch without screaming “WHY” at the TV screen.
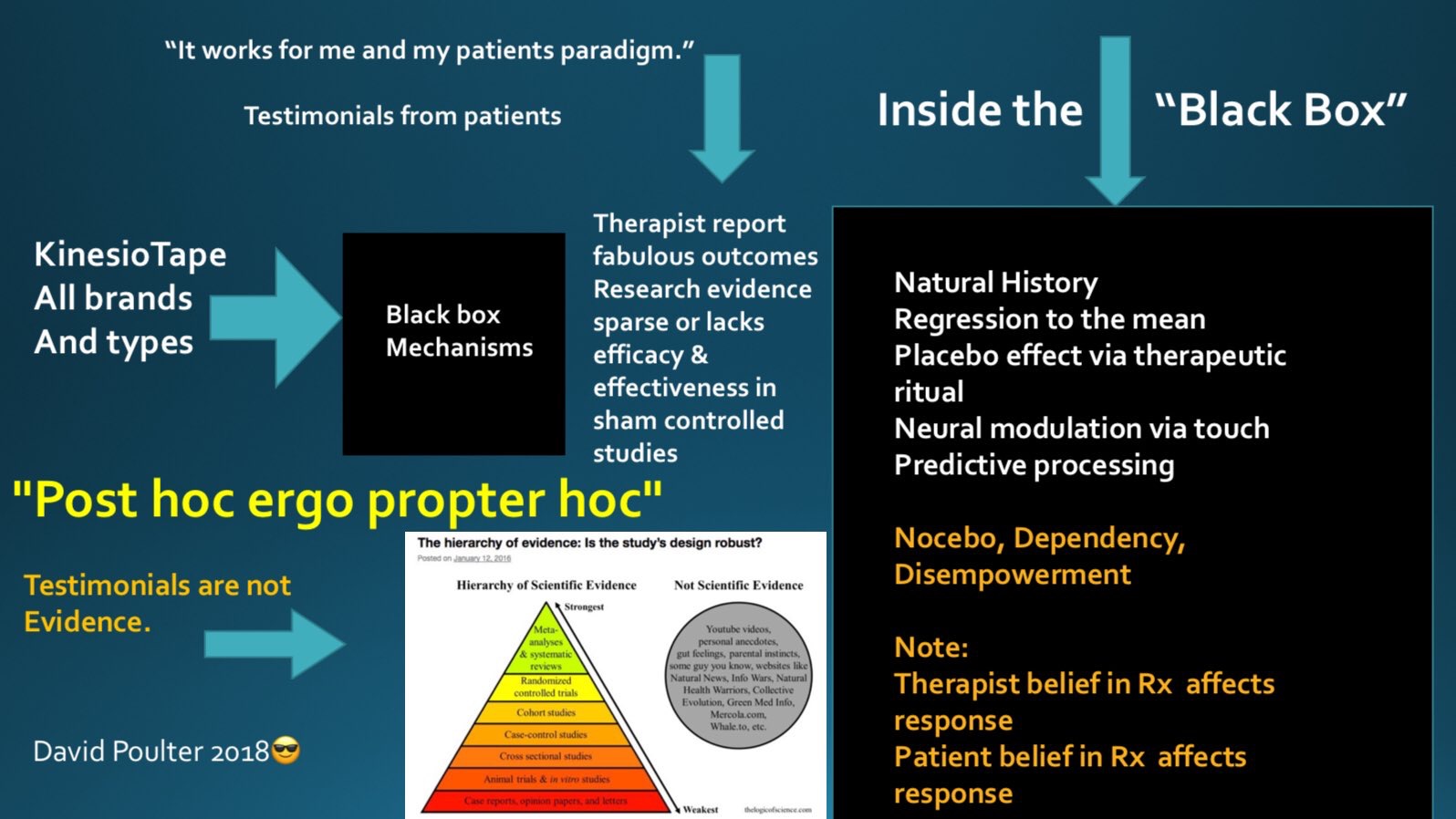
My thoughts questions and reflections:
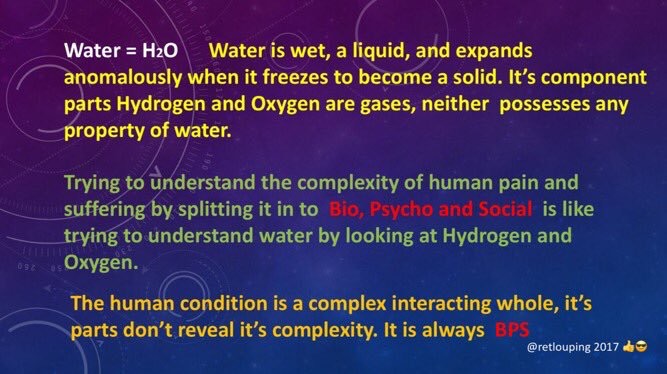
- Pain should be respected, sometimes it is due to damage and you can’t out exercise it.
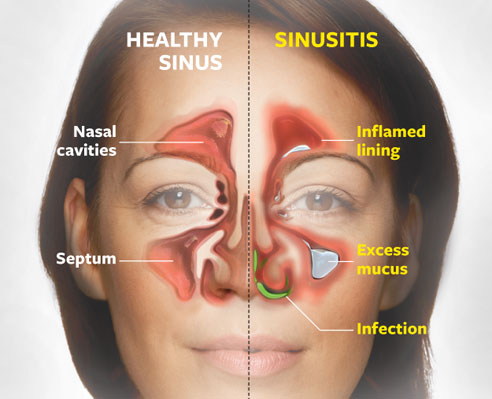
- You can’t cut out pain and just because you see things on MRI, fixing them may not solve the PAIN problem.
- Is passive stretching into pain in early post op care indicated?
- Did the rehab team understand post op labral repair ROM restrictions and recovery timelines?
- You can do too much loading to soon post operatively.
- You can’t cut, burn or inject away pain.
- should you inject corticosteroids into a hip with severe articular cartilage changes? (See twitter discussion in article)
- You can’t accelerate healing by exercising excessively.
- Each new health care provider offers hope, which can be quickly dashed when pain and function don’t improve as promised.
- You can be too close to a patient to give them advice.
- Twitter pundits advice is sometimes the wrong advice in certain situations. ie hurt doesn’t mean harm, you can’t go wrong getting strong, you can exercise with pain, your scan isn’t your destiny, exercise is the answer………etc, etc, etc
- Rest is sometimes indicated.
- Your rehab team should not be your friends?
My early comments from twitter:
“Just finished watching, have to admit it brought some Tears to my eyes. A powerful, powerful lived experience narrative.
My only comment is that his medical support team need to watch & do some self reflection.
You can not keep smashing your head against a wall and expect no pain”
“Watching Andy Murray Resurfacing whilst I spin. 🚴🏻
It is so hard to watch. Easy to second guess in hindsight.
Current thoughts.
- You can’t cut out pain.
- You can’t ignore some pains, they do mean damage.
- Why do PTs stick their elbow in people’s butt cheeks?”
Below is a general review of the documentary
The Gist: For the uninitiated, Murray is one of the greatest male tennis stars ever (a surefire Top 20 player ever), and has a list of accomplishments from here to the moon. But by 2017, a dozen years into his pro career, early retirement was looking like a serious possibility. He suffered a hip injury requiring rehabilitation. And then, surgery. And eventually, surgery again. That last surgery looked like it might be just-so-he-can-walk-normally surgery, not play-gruelingly-intense-tennis-matches surgery. He was 30 years old at the time, which is getting-up-there for a pro tennis player, but it’s not a decrepit age where he’d be better off shuffling to the park to play chess with the geezers.
Amidst all this was incredible indecision — and who can blame him, considering the blooms of uncertainty burst with vivacious color as we grow older? As many sports stars tend to be, Murray is a guarded individual, which makes director Olivia Cappuccini’s access here notable. She hangs with him during countless rehab and workout sessions, scenes that don’t seem quite so tedious when we realize Murray endured 1,000 more that weren’t caught on camera. We get glimpses of him in his mansion with his wife, Kim — a frequent talking-head commentator — and their toddler children; we see him weep during a press conference before a match that might be his last; we’re all-too-present for the gory details of the second surgery, where he had the ball of his hip replaced with metal.
Why does Murray so desperately need to continue? Tennis is all he knows: Cue the old snapshot of him as a grade-schooler, holding a racket and grinning. There’s also the therapeutic component. For his most psychologically raw and intensely human moment, he’s not on camera, but audio only, sharing how his mother used to give rides to a man that eventually shot up his school while he took cover in a classroom; how his parents divorced soon after; how his older brother, with whom he was very close, moved away. Tennis helped relieve him of his anxiety. So maybe now we know why he’s so animated and passionate on the court, and so reluctant to give up the thing that gave him not only great joy and great pain, but also escape and catharsis.
https://decider.com/2019/12/04/andy-murray-resurfacing-on-amazon-prime-stream-it-or-skip-it